|
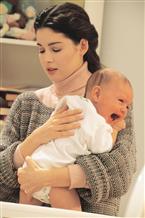
 Part 1 - I'm So Happy I Could Cry: The Truth About Postpartum Depression Part 1 - I'm So Happy I Could Cry: The Truth About Postpartum Depression
 Save to notebook Save to notebook
 Email article Email article
 Print article Print article
 More articles More articles
 You must first be logged in to edit a post.
If you are not registered, please click "Create Account". By Mia Bolaris-Forget
For many couples having a baby is the consummate consummation or their love and commitment to each other and to their future. In fact, for “traditional” marrieds it is the “logical” next step in a (literally) growing relationship. But beyond the (initial) excitement of the blessed news, the morning sickness, the hormone fluctuations and the inevitable bulging belly and motion of the child you are housing, there are other (not-so-obvious) changes taking place. Among these, the transition from couple to family and adjusting to the idea that you are, or soon will be a parent, responsible for the life and decisions of someone else. And, like any new transition, it takes some time to adjust and get use to….even for those who may have been down this road before.
While your heart is beating excitedly at the prospect of welcoming (home) your new (family) member and embracing your new role and responsibility pouring love and libations over your dear little one, your head is beating, or should I say pounding uncontrollably, fiercely out of control with thoughts you thought would never cross your mind…at least in as a “sane” individual. You (or maybe someone you know) has become more easily irritable, emotional, and anxious. You are either ravenously hungry or not hungry at all, are increasingly apathetic and lethargic (though you may often experience trouble relaxing or sleeping)… and the thought of life with your new child has become a damning sentence rather than an event to look forward to.
You are going “crazy” or so you believe, and your behavior seems to be pushing (even those closest to you) away….validating your feelings of loneliness and being alone. But, mommy dearest, you are NOT alone…and so, according to the experts, you should not be during this very important and sensitive time in your life and pregnancy.
Singing The Blues (And The Blahs):
Defining Depression:
Depression is classified as experiencing “unjustified” doldrums for extended an extended period of time. While it is not uncommon for individuals to feel sad, unhappy or “out of whack” once in a while, prolonged periods of sadness, frustration, listlessness, and detachment interfering with daily life, “social etiquette” and responsibility may evoke concern and require (medical) attention and a re-direction in life skills and thinking.
Frequency and Occurrence:
“Erratic” emotions and the onset of “depression” during pregnancy and up to a year after delivery is known as perinatal depression. While statistics are vague as to the exact amount of pregnant women who suffer from these symptoms, statistics show that these symptoms are quite common among women. According to studies and research this may occur (and often go undiagnosed and unattended) not only because of the “natural” stress associated with the realization of your new role, but also because of actual hormone and other “normal” pregnancy changes simultaneously occurring through pregnancy and into the first few weeks after delivery.
Attributing and Contributing Factors:
As with anything NEW in life, it always looks better on paper (or in our mind). Reality is quite a different story, and even the most glorious and advantageous, even planned for and eagerly anticipated event may require a bit of acceptance and adjustment. Life-altering experiences and situations generally do…and that inevitably implies “stress”. How we perceive and react and respond to that stress, along with congenital hormone and chemical changes can aggravate and already delicate situation, though exact causality cannot be determined.
Pregnancy Blues:
While pregnant a woman may “attribute” bouts of depression to the following:
· History of depression or substance abuse
· Inherited/Learned reaction, response and behavior
· Lack of support (from family and friends)
· Concern and anxiety about the fetus
· Problems conceiving or with previous pregnancy or birth
· Marital or financial issues
· Lack of (mental and/or chronological) maturity (of mother
Post Pregnancy:
The most commonly recognized and experienced form of the “baby blues”, known as postpartum or peripartum depression. During the gestation period a woman’s body goes through a mélange of hormonal changes including a significant increase in levels of estrogen and progesterone. Yet, these hormone levels return to normal just 24 hours after childbirth. So, researchers seem inclined to believe that this rapid fluctuation in hormone levels may potentially contribute to feelings of depression, similarly to how smaller fluctuations reflect a mood change during a woman’s menstrual cycle.
Additionally, experts note that thyroid hormones also seem to plummet after childbirth. The thyroid is a small gland in the neck that moderates metabolism and how our bodies use and store food energy. Low thyroid levels may lead to symptoms of depression including sadness, loss of interest in life and generally enjoyable activities, irritability, fatigue, lack of concentration, sleep apnea, and weight gain. A simple blood test can test for this condition, and medications are available by prescription.
Other influences that may trigger this condition include:
· Post delivery fatigue, varied sleep patterns, and lack of adequate rest, which may all, contribute to the inability to regain necessary and essential strength.
· Feeling of doubt about your parenting skills and abilities, or simply being overwhelmed with your new added responsibility.
· Stress due to changes in daily routines. Self-imposed (perhaps impractical) expectations.
· Feeling of loss. Loss of identity, control, or of your pre-pregnancy figure…and perhaps feeling less attractive.
· Struggles with time management. Having less time and less “control” of time, being confined to your home more often, and having less time for personal pleasures or for spending time with friends and loved ones.
Timing Is Everything:
Experiencing the “baby blues” does NOT automatically mean you are suffering from postpartum depression. In fact, professions suggest that an attitude adjustment is a natural part of the pregnancy process. Although there is no specific timeline for officially “diagnosing” someone as clinically depressed (after childbirth) experts agree that most women tend to feel better within a few weeks, while others may take a bit longer. They emphasize that women who have a history of depression or whose symptoms are severe and longer lasting should air on the side of caution and seek out a professional diagnosis and professional help.
Signs of the Time:
According to authorities, symptoms lasting longer than two weeks are warning signs for depression. They suggest looking out for the following:
· Restlessness or irritability
· Sadness, hopelessness and feelings of being easily overwhelmed.
· Frequent (and unwarranted) bouts of crying.
· Lack of energy or motivation.
· Drastic changes in diet (eating too little or too much)
· Erratic sleep patterns (sleeping too little or too much)
· Anti-social behavior and withdrawal from friends, family, and obligations
· Experiencing headaches, chest pains, heart palpitations, or hyperventilation.
Post pregnancy depression may also include anxiety about hurting the baby or oneself and/or lack of interest in the child.
The Three “Stages” of PPD:
1. The “Baby-Blues”: Generally occur in the first few days following pregnancy…and “disappear” just as quickly as they appeared (usually within a week or two). Most mom’s going through the “baby blues” experience sudden mood swings, sadness, crying fits, loss of appetite, sleeping disorders, restlessness, anxiety, and loneliness. Symptoms are fairly mild and there’s no need for treatment. Professionals suggest alleviating symptoms by napping when the baby does, seeking help from friends and family, and joining a support group.
2. Postpartum Depression: Typically occurs within the first year after giving birth. A woman may experience a variety of symptoms including sadness, loss of energy, lack of concentration, anxiety and feelings of guilt and worthlessness. The primary difference between the “baby blues” and postpartum depression is that the latter frequently affects the woman’s ability to function normally, impedes on her health and well-being, and lasts substantially longer. Additionally, postpartum depression is classified as a significant condition requiring medical attention often including counseling and possibly medication.
3. Postpartum Psychosis: A rare condition affecting 1 or 2 out of every 1000 births and generally occurs in the first 6 weeks after childbirth. Women who are considered bipolar or have other psychiatric conditions are at higher risk for this “disorder”. Symptoms may include delusions, hallucination, erratic sleep patterns, and obsessive thoughts about the baby. Additionally, a woman may go through rapid mood swings, from depression to irritability, to mania and euphoria.
From Postpartum to Attention Deficit:
Many women battling their feelings and thoughts after childbirth often go neglected. Because they are frequently ashamed, embarrassed or feel guilty, act in ways that push friends and family aside, and put themsleves at risk for NOT getting the attention, support, and guidance they so desperately need.
What needs to be realized is that postpartum depression is NOT a negative reflection of you (as a person or a mother). It is simply a situation that you need to learn to accept, handle and effectively control, and which often requires the help of others. We all have “weaknesses”, “difficulties”, “fears”, and “anxieties”…what’s most important is showing the strength of our character but NOT be ashamed of them, but learning about ourselves from them and effectively confronting and addressing them so that they DON’T interfere with our lives, obligations, relationships and potential (accomplishments and achievements). I’m sure most would not hesitate to ask for assistance at a new job (even if we’d done that job before…after all every company has it’s own policies right?); nor would we be ashamed of asking someone’s opinion on a new hairstyle or outfit, eliciting help with a new recipe, seeking out company to share a long drive with, or taking our time getting adjusted to driving a new vehicle. Having a baby IS a major life event and should be no different. In fact, the best gift you can give to yourself, your baby and your family is recognizing your feelings and taking action toward a better, more productive, and happier future.
Consult your doctor or midwife if you are having any symptoms of depression during or after pregnancy. They can prescribe a questionnaire to test for depression and put you on the right road to recovery.
Some pragmatic pointers include:
· Rest and relax as often as possible. Consider down time along with the baby and that includes naps.
· Take it easy! Take additional pressure off yourself by convincing yourself that you can accomplish as much as you did before your baby. Do what you can and leave the rest.
· Ask for assistance. Consider getting help from your partner, friends, and family with everything from household chores to nighttime feedings. If financially feasible, leave laundry and housecleaning to the professionals…and order in (making sure its healthy, nutritious, and lean) as often as you can.
· Discuss your feelings with your partner, friends, and family…or seek out a support group or a professional you trust and are comfortable with. If funds are an issue consider a group at your local church or temple.
· Get up and out. The less time you spend alone, the better. Hook up with other moms, visit family and friends or simply go window-shopping or run errands. Remember to “dress up”, do your makeup and leave the house feeling good about yourself….even if you only go for a short walk.
· Get a baby sitter or leave your new baby with a friend or family member once a week and get out with your spouse. Decide on a time to put the baby down so you and your partner have adult time alone.
· Keep in touch and stay in the loop. Do volunteer work or get a home-base part time job to keep you and your mind occupied. Talk with other mothers and ask for advice and helpful hints you can learn from…maybe consider asking YOUR mom for advice.
· Join a support group for women with depression. Contact a local hotline or peruse the telephone book for information and services.
· Refrain from making additional major life choices (if possible). Major changes may evoke stress. If you can’t avoid additional stressors, arrange for support and help ahead of time.
Well-Care and Treatment:
Authorities agree that the primary focus of PPD is the well-being of the mom. Besides pampering and understanding there are typically two common types of treatment for such conditions:
· Talk Therapy: Probably the best, first “alternative”, involving speaking to a professional (therapist, psychologist, or social worker) to learn about changing your thought process, behaviors and reactions.
· Prescription Remedies: Medicines such as antidepressants may be required fro more sever cases and prolonged symptoms.
Pregnant or breastfeeding women should consult their physicians before taking prescription drugs. Concerns may include medicinal effects on the baby. While a valid “fear”, it’s also important to realize that NOT taking action may be equally as “hazardous” to your child and his/her development.
Avoidance Behavior:
Giving yourself enough time to heal mentally and physically during and after childbirth should always be the first course of action. Still, untreated, persistent symptoms should NEVER be dismissed or avoided. In fact, mental “disturbances” should be treated with the same urgency as physical ones ….and may pose a threat to both you and your baby.
Depression during pregnancy may increase the risk of delivering an underweight or premature baby. Furthermore, some women experiencing emotional difficulties may face trouble taking care of themselves (hence also “neglecting” their infant). They may have trouble eating, sleeping, miss prenatal visits, fail to follow medical instructions, have poor eating habits, and/or indulge in harmful practices such as smoking, drinking, or using illegal drugs.
Postpartum depression, because it affects judgment, may inhibit a mother’s ability to appropriately care for her child. She may be energy deficient, lack concentration, be irritable and fail to meet her infant’s needs for love, attention, and affection (especially she is in desperate need for these things herself). Her condition may also lead to guilt and shame, a loss of respect and confidence from others and herself…and THIS can worsen the initial problem. According to studies, mom’s who experience postpartum depression and an inability to correctly care for their child may also “impose” on the child “developmental disadvantages” including: delays in language development, problems with emotional bonding with others, behavioral problems, lower activity levels, sleep “disorders”, and distress. They suggest dad or any other caregiver taking a visible role in addressing the need of mother and baby alike, especially during this delicate time in their lives.
Next: Doctor, Doctor: Turning To Your Doctor For Help >>
Long Island Health, Fitness & Beauty Articles
>
Part 1 - I'm So Happy I Could Cry: The Truth About Postpartum Depression
|


Long Island Bridal Shows
|










